Introduction
In this article, we will explore the construction and optical layout of both the retinoscope and the ophthalmoscope, highlighting their unique designs and functionalities. Understanding these differences is crucial for professionals looking to select the most suitable tool for precise eye examinations. Whether you are focusing on the improved accuracy of a retinoscope or the advanced visualization capabilities of an ophthalmoscope, we will guide you through the essential aspects of each device.
Retinoscope Design
Retinoscopes are a very common optical instrument used by optometrists to examine a patient’s eye and evaluate the need of corrective lenses. They use a very interesting physical principle.
Let’s first describe the optical instrument. This is a handheld device that the optometrist places right in front of their eyes. It projects a slit into the patient’s eyes, and the optometrist observes the red reflex that illuminates the pupil to determine the required accommodation for the patient. The red reflex is what we usually think of as ‘red eye’ when taking a picture with flash.
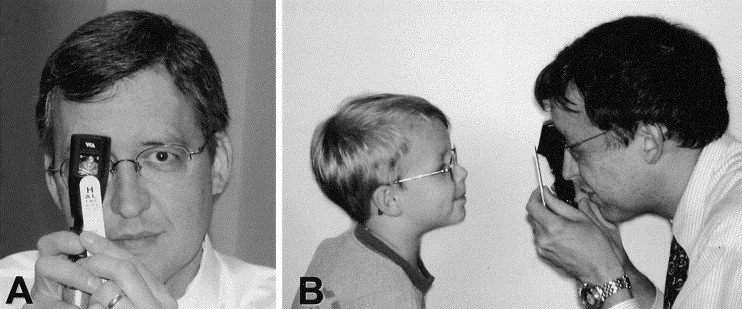
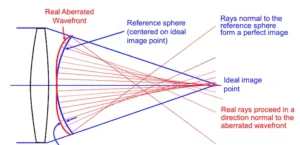
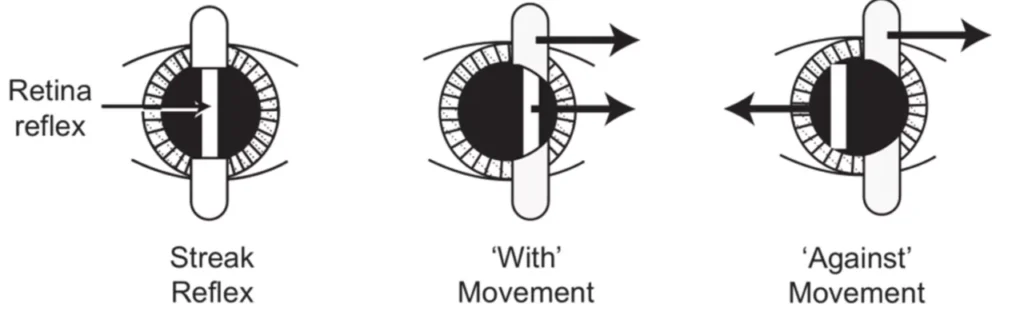
Figure 1 shows the use of a Retinoscope from the patient’s point of view (A) and a lateral view (B). Image from Survey of Ophthalmology
By rotating the device, the slits are moved across the pupil. If the patient’s far point lies behind the observer’s eye, the observer will see that the red reflex moves in the same direction as the motion of the slit. This movement is called ‘with motion.’ Likewise, if the patient’s far point lies between the observer and the patient, the red reflex will move in the opposite direction to the slit’s movement (or ‘against motion’). Finally, when the patient’s retina is conjugate to the device, there will be motionless uniform illumination (also called ‘point of neutrality’).
The optometrist can place lenses with different powers in front of the patient’s eye until the optometrist find the point of neutrality.
Optical design of the Retinoscope
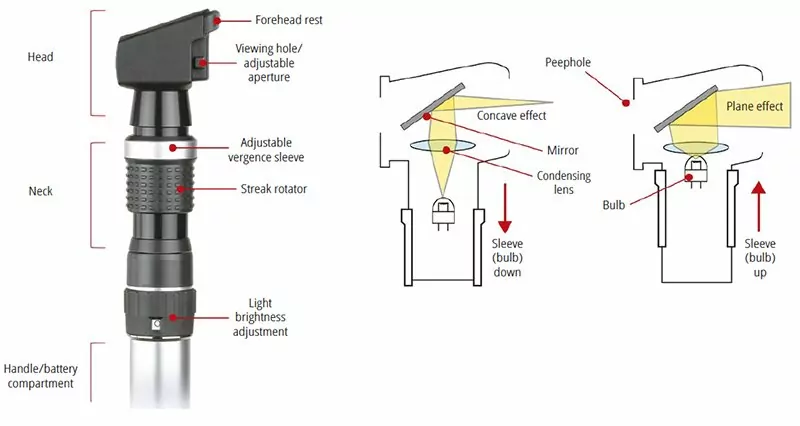
From the point of view of optical design. A basic retinoscope can have a very simple configuration. It will have a light source, lens, and a movable barrel that can change the distance between the source and the lens. Additional elements include cards with the slit profile and focusing cards that helps the patient direct their sight into the device.
Retinoscopes are very useful when working with small children. Because it’s a less subjective test and less intimidating that using a traditional Phoropter.

Ophthalmoscope Optical Layout
Here, we will talk about the different instrumentation used by ophthalmologists and optometrists. As you can imagine, there are many restrictions when designing an optical instrument that will be used in a patient. It matters whether the instrument is meant to be used as a diagnostic tool or during surgery, and whether the patient is awake or unconscious.
Here, we will focus on optical instruments used in the diagnosis and evaluation of some human eye parameters. Some of you may have already encountered them during a regular eye exam.
For today’s entry, we will talk about one of the most basic optical instruments used by optometrists and family doctors: the funduscope. This instrument allows the doctor to see the back of the eye. They can observe the retina, the optic nerve, the macula fovea, and the vascular system (all these structures are sometimes referred to as the fundus of the eye). By looking at these structures, a doctor can diagnose different ailments like endocarditis, diabetes, glaucoma, separation of the retina, and hypertension.
There are three models of funduscopes: classical, panoptic, and indirect funduscope (that looks like a miner’s light). The first two are shown in Figure.

Optical Design
A funduscope consists of 3 essential elements: a light source, a mirror or beam splitter that redirects the light to the eye, and an optical means of correcting a non-sharp image of the fundus. In reality, they can be more complex. You normally want to control the amount of light and the size of the light source to adapt the light cone that goes into the patient’s eye.
In addition, you may need different colors of light source to enhance contrast or identify retinal lesions. Some instruments include grids as a basic measurement between retinal features. In order to correct the non-sharp fundus image, one can use a wheel of lenses with different powers or a movable lens that allows focusing at different points. An image of the instrument is shown in Figure 2.
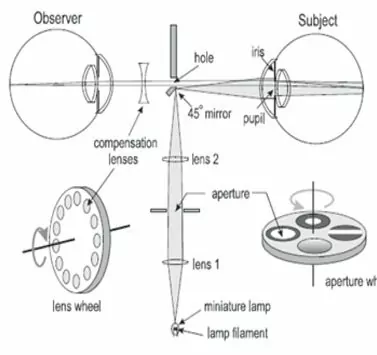
Image from Delhi Journal of Ophthalmology
Finally, I would like to mention that when performing a test, an optometrist may require you to dilate your pupils. This is not always the case but it will depend on how much of the retina they need to observe.
Non-Contact Tonometers
This article concludes our exploration of optical instrumentation for optometry. If you’re new to this topic, I recommend checking out the sections on Ophthalmoscope Design, Keratometer Design, and Retinoscopy, which provide valuable insights into other key optometry tools. This week, we will talk about a very interesting optical device that uses the mechanical properties of the eye to make a measurement.
Internal ocular pressure is measured with non-contact tonometers, which aids in the diagnosis of glaucoma. The method of measurement is pretty intriguing. The patient is subjected to an air pulse that distorts the shape of his or her eye. The amount of distortion and the time it takes for the eye to return to its natural shape are then monitored using infrared light.
To fully comprehend this technology, we must first examine the biomechanics of the cornea. The cornea is depicted schematically in Figure 1.
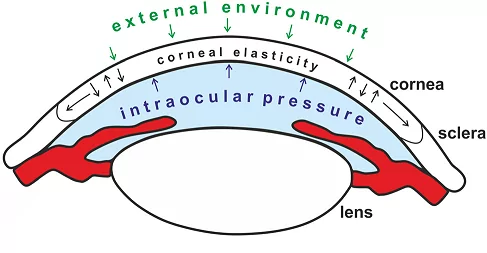
Many biological tissues, including the cornea, have viscoelastic qualities. That is, depending on the rate at which a force is delivered, it will react differently. The so-called Newtonian Fluids, which a person can walk over if they move quickly or sink if they travel slowly, are another viscoelastic material that many readers may be familiar with.
The non-linear behavior of viscoelastic materials is an important factor to consider. When it comes to the cornea, The stress–strain curve can be broken down into sections to show changes in collagen organization during stress. The viscous reaction of ocular tissue is dominant at low distortion, whereas the elastic response is dominating at big deformation.
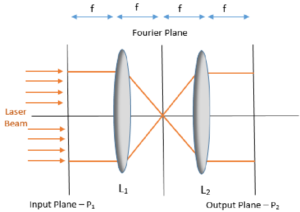
Due to copyright constraints, details on a commercial non-optical tonometer are difficult to come by. The fundamental layout of a non-contact tonometer is shown in Figure 2. As you may expect, we have two distinct systems. One is mechanical, which controls the puff of air, and the other is optical, which handles the measurements. We need to be able to manage the force and speed of air release for the air-puff, but we won’t discuss that mechanism here (this is an optic blog, after all).
A light source (typically infrared/visible), image optics, a photodetector (PD), and a position sensing detector are among the optical components (PSD). The cornea is in what is known as a “applanation state” after the air puff has been released. The cornea’s front portion flattens out like a mirror, reflecting the maximum amount of light from the lightsource into the PD.
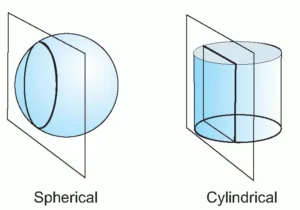
This will be visible as a peak in reflection that gradually fades as the cornea returns to its original shape. The PSD was utilized to determine the corneal strain. To account for the image deformation caused by the light source and detectors being off-axis, we’ll require a cylindrical lens.
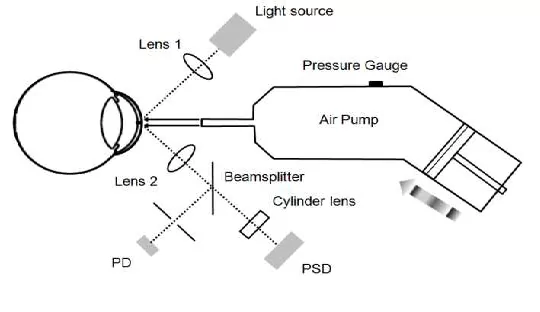
A photodetector (PD) and a
Position sensing detector (PSD) are syed to monitor the status of cornea applanation and the
cornea displacement, respectively. Image after Wai W Wang et al.
Non-contact tonometers are widely used, although they are not the only method for measuring intraocular pressure. Commercially available methods include the Ocular Response Analyzer (ORA) and Corneal Visualization Scheimpflug Technology (Corvis CT). Because of its imaging speed, noncontact nature, and high image quality, optical coherence elastography (OCE) has a lot of clinical potential.
Conclusion:
Function: A retinoscope is used to measure refraction and assess vision needs, while an ophthalmoscope is designed for examining the internal structures of the eye, including the retina, optic nerve, and blood vessels.
Application: The retinoscope aids in determining the appropriate vision correction, while the ophthalmoscope is essential for diagnosing eye conditions such as glaucoma, retinal detachment, and other retinal diseases.
Method of Operation: The retinoscope assesses the reflection of light from the retina to determine the necessary lens prescription, while the ophthalmoscope provides a direct visual inspection of the interior of the eye.
In summary, the retinoscope is primarily used to measure refractive errors, while the ophthalmoscope offers a detailed view of internal eye structures for diagnostic purposes. Combined with non-contact tonometers, these tools provide a comprehensive approach to eye examination and care.